Protecting Your Vision with Care and Precision
Your eyes are one of your most important senses, and keeping them healthy helps you stay connected to the world around you. At Advanced EyeCare & Aesthetics, we provide personalized care for every stage of eye health, from routine checkups to managing serious conditions.
Whether you’re experiencing dry eye, noticing changes in your vision, or managing a chronic eye condition, we take the time to understand your needs and create a plan that works for you.
Using diagnostic technology and proven techniques, we focus on preserving your vision, supporting your eye health, and helping you feel confident in your sight. Let’s take charge of your eye health together. Book an appointment with us today.


Our Approach to Eye Exams
We provide in-depth eye exams using our diagnostic technology to get a complete picture of your eye health. This allows us to detect issues early and create personalized treatment plans tailored to your needs.
Our goal is simple: to help keep your eyes healthy, maintain sharp vision, and create an experience that is seamless and supportive.
Our Diagnostic Testing
We’re proud to have a suite of reliable technologies to test for various eye diseases. Our diagnostic technology includes:
- Heidelberg OCT testing: This detailed, noninvasive imaging test helps us precisely diagnose and manage various eye diseases, including glaucoma, age-related macular degeneration, and diabetic retinopathy.
- Optos retinal imaging: This noninvasive imaging technology captures a wide view of the retina in 1 image to help with early detection and monitoring of eye conditions.
- Dilated fundus exams: For this test, eye drops are used to enlarge the pupil, allowing for a detailed examination of the retina and optic nerve. This test helps us detect and monitor eye diseases like diabetic retinopathy, macular degeneration, and glaucoma.
- Wavefront Corneal Analysis: Uses detailed mapping of the cornea to detect subtle irregularities, helping identify early signs of eye conditions and guide personalized treatment plans.
- Virtual Reality Visual Field Testing: Uses VR technology to assess peripheral and central vision, helping detect early changes from glaucoma, retinal disease, or other visual field disor
Cataract Management
Cataracts are cloudy spots that form in your lens, leading to blurry vision and difficulty seeing clearly. This condition typically develops with age but can be influenced by other factors and certain medical conditions, such as diabetes.
Surgery may be required to remove the cataract in your eye and replace it with an artificial lens to restore your vision. You can reduce your risk of developing cataracts by:
- Wearing sunglasses with full UV protection
- Quitting smoking
- Following a healthy diet
AMD Management
Age-related macular degeneration (AMD) can affect people differently, and you may not notice any changes in your vision early on, which can make AMD hard to spot without an eye exam.
There are 2 types of AMD, wet and dry. Dry AMD is more common and tends to develop gradually. Wet AMD can develop suddenly and may require prompt treatment.
As the condition progresses, the range of symptoms you might experience can include:
- Difficulty reading
- Distortion or bends in what should be straight lines (such as lampposts or door frames)
- Dark spots in your central vision
- Fading colors
- Poor night vision
- Blurred vision
- Objects appearing to change shape, size or color, or moving and disappearing
- Light sensitivity
AMD Prevention and Treatment
You can take steps to support your eye health and lower your risk of developing AMD:
- Quit smoking
- Eat a healthy, balanced diet rich in fruits and vegetables
- Moderate alcohol consumption
- Maintain a healthy weight
- Get regular exercise
There is no cure for AMD, but treatments can help preserve vision and manage symptoms. For dry AMD, the focus is on supporting and maintaining your sight, which may include lifestyle adjustments or tools such as magnifying glasses for reading.
Wet AMD can be treated with medications that slow disease progression, and in some cases, laser therapy may be an option. Your eye doctor will help determine the best treatment approach based on your specific needs.
Diabetic Eye Disease
Diabetes occurs when the body is no longer able to regulate its own blood sugar levels and requires intervention to keep them stable. Many people are surprised to learn that having diabetes can also affect their vision.
Diabetes can damage the blood vessels in your eyes, leading to conditions like diabetic retinopathy. Without treatment, diabetic retinopathy can cause vision loss. Diabetes can also increase your risk of developing other eye conditions. For those reasons, people living with diabetes are strongly encouraged to get regular diabetic eye exams.
What to Expect from Diabetic Eye Exams
Diabetic eye exams are noninvasive. During the exam, you will be given eye drops, which will dilate your pupils and blur your vision. Once your pupils are wide enough, you will be asked to rest your head on a device and look into a camera that will take images of the back of your eyes.
You will see a flash when each image is taken. Using those images, we can assess the structure of your eyes, including the retina, and look for any abnormalities.
In addition to the images of the back of your eye being taken, you will also be given a visual acuity test to help us assess the clarity of your vision and monitor the effects that diabetes could be having on your sight.
Glaucoma Management
Glaucoma is a group of eye diseases that can damage the optic nerve and lead to vision loss. It is often associated with high eye pressure, but it can also occur at normal or low pressure.
There are several types of glaucoma, including:
- Open-angle glaucoma
- Angle-closure glaucoma
- Normal-tension glaucoma
Risk factors include age, family history, high eye pressure, thin corneas, and certain medical conditions. Because glaucoma can develop subtly, regular eye exams are essential for early detection and prevention.
Assessing Your Risk
During your eye exam, we evaluate your risk for glaucoma by:
- Measuring your eye pressure
- Asking about family history and medical conditions
Considering your vision type, farsightedness can increase the risk of narrow-angle glaucoma, while nearsightedness can increase the risk of open-angle glaucoma.
Standard Glaucoma Testing
We check for glaucoma at every comprehensive eye exam to establish a baseline and monitor changes over time. Standard tests include:
- Tonometry: Measures eye pressure using a gentle puff of air after numbing drops. Eye pressure is just one piece of information we use to assess your eyes.
- Ophthalmoscopy: Allows us to examine the shape and color of your optic nerve in detail. Drops are used to dilate your pupils, making it easier to see the back of the eye.
Additional Glaucoma Testing
Depending on your results, we may recommend additional tests:
- Perimetry: Maps your full field of vision. You’ll respond when you see moving lights in your peripheral (side) vision. Accuracy may require repeating the test.
- Gonioscopy: Examines the angle between your iris and cornea using a handheld lens to determine if fluid drainage is blocked or open.
- Pachymetry: Measures cornea thickness to help interpret eye pressure readings and confirm glaucoma diagnosis.
Helping You Navigate Eye Disease
Your eyes are priceless, and staying on top of your eye health is one of the best ways to protect them. At Advanced EyeCare & Aesthetics, we provide thorough exams, testing, and personalized care plans for conditions like glaucoma, macular degeneration, cataracts, and diabetic eye disease.
We take the time to understand your needs and guide you toward treatments that preserve your vision and support your overall eye health. Regular checkups, early detection, and proactive care can make a real difference in maintaining clear, comfortable vision for years to come.
Book an appointment today and take the next step toward protecting your vision. While you are here, consider exploring our medical aesthetics and wellness services to look and feel your best.
Our Services
Come Visit Us in Plymouth
We are located on the northeast corner of East Mill Street and North Stafford Street. We have ample parking, including accessible parking spaces, and a wheelchair-accessible entrance at the rear of the building.

Our Address
- 300 East Mill St.
- Plymouth, WI 53073
Contact Information
- Phone: 920-893-8474
- Fax: 920-893-8814
- Email: contactus@advancedeyecareplymouth.com
Our Hours
- Monday: 8:30 AM – 6:00 PM
- Tuesday: 8:30 AM – 6:00 PM
- Wednesday: 8:30 AM – 5:00 PM
- Thursday: 8:30 AM – 5:00 PM
- Friday: 8:30 AM – 4:00 PM
- Saturday: By Appointment Only
- Sunday: Closed
Our Brands
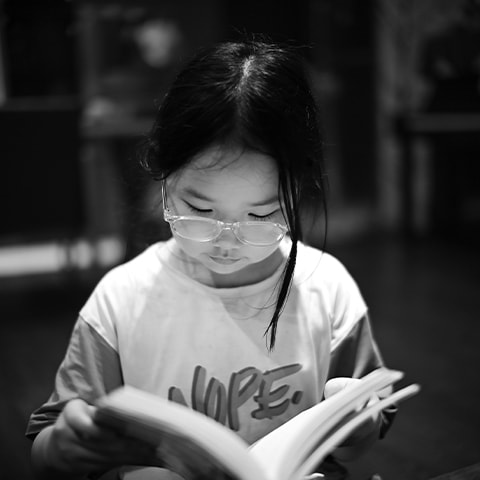
Discover a blend of style, comfort, and clarity with our extensive collection of eyeglass frames and lenses.
Whether you’re seeking the durability and flexibility for everyday wear or the luxury and elegance for special occasions, we have you covered.
Embrace quality. Enjoy clarity. Experience Advanced EyeCare & Aesthetics.